Introduction
Alopecia areata (AA) is an autoimmune, non-scarring hair loss disorder characterized by localized, patchy hair loss. Although scalp involvement is most common, beard alopecia areata (BAA) is increasingly recognized as a distinct presentation that affects quality of life, self-image, and social confidence—especially in young male patients. The disease course is unpredictable, with spontaneous regrowth in some and chronic relapsing patterns in others. A multi-modal, individualized treatment approach is often required.
Case Presentation
A 37-year-old male presented with a 3-week history of patchy hair loss in the beard region, predominantly on the right mandibular and submandibular area. The patient denied prior episodes, recent illness, major stressors, or family history of autoimmune disease.
Clinical examination revealed well-demarcated, smooth, non-scarring alopecic patches with preserved follicular openings, consistent with Alopecia Areata – Beard Variant. Dermoscopy showed yellow dots, exclamation-mark hairs, and tapered broken shafts supporting the diagnosis.
Dermoscopic Findings
- Yellow dots: Hyperkeratotic plugs in empty follicular openings
- Exclamation-mark hairs: Characteristic tapering at proximal end
- Tapered broken shafts: Evidence of structural hair shaft weakness
- Preserved follicular architecture: Non-scarring nature confirmed
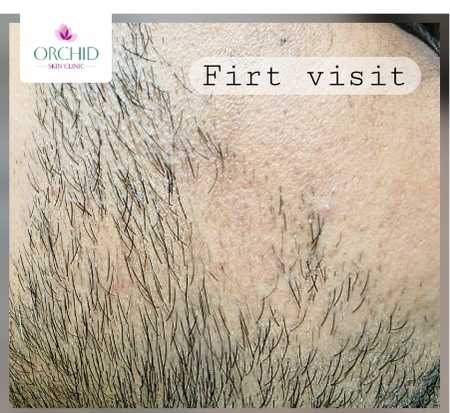
Baseline - First Visit
Well-demarcated alopecic patches in right mandibular region with smooth, non-scarring appearance and preserved follicular openings.

4-Week Follow-up
Significant regrowth with visible pigmented terminal hairs and marked reduction in patch size following multi-modal therapy.
Diagnostic Approach
Clinical Diagnosis
Diagnosis was based on:
- Clinical appearance: Localized smooth patches
- Dermoscopy findings: Yellow dots, exclamation-mark hairs, tapered broken shafts
- Absence of scarring: No scale, atrophy, or scarring
Differential Diagnoses Ruled Out
- Tinea barbae: No scaling, no erythematous border
- Trichotillomania: Lack of irregular broken hairs
- Frictional alopecia: No history of mechanical trauma
- Scarring alopecias: (e.g., FFA, LPP) – not consistent with clinical examination
Baseline investigations (CBC, LFT, TFT, Vit-D) were normal. No evidence of associated thyroid or autoimmune disease.
Pathophysiology
Alopecia areata is believed to result from a T-cell mediated autoimmune attack on anagen hair follicles. Collapse of immune privilege in the bulb triggers:
Immunopathogenesis
- CD4+ and CD8+ T-cell infiltration: Periand intrafollicular inflammatory infiltrate
- Upregulation of interferon-γ: Key cytokine in disease pathogenesis
- JAK-STAT pathway activation: Downstream signaling cascade
- Arrest of anagen phase: Premature catagen transition with sudden shedding
Beard AA is sometimes associated with local trauma ("reverse Koebner phenomenon"), genetic factors, or stress-related immune dysregulation.
Treatment Approach
The patient underwent a multi-modal, staged therapeutic plan:
Intralesional Steroid Therapy
- Triamcinolone acetonide 10 mg/mL (1:1 dilution)
- Injected intradermally at 0.1 mL per point, spaced 1 cm apart
- Repeat session planned at 3–4 weeks
Oral Pulse Steroid Therapy
- Weekend oral betamethasone pulse for 4–6 weeks
- Aims to suppress acute autoimmune activity and halt progression
Topical Therapies
- Topical clobetasol propionate 0.05% once daily (2 weeks on, 1 week off)
- Topical tacrolimus 0.1% ointment at night for immune modulation
Adjunctive & Future Options
Discussed with patient for potential escalation in case of poor response:
- Excimer laser (308 nm): 2–3 times weekly to stimulate regrowth
- Contact immunotherapy: DPCP/SADBE for resistant cases
- Topical minoxidil 5%: To enhance regrowth
- Oral JAK inhibitors: (e.g., tofacitinib)
- Highly effective for extensive AA
- Acts via JAK-STAT inhibition
- Requires monitoring for infections/liver enzymes/lipids
- Platelet-rich plasma (PRP): As an adjunct modality
- Systemic immunomodulators: (methotrexate, cyclosporine) for refractory disease
Clinical Course
At the second visit (4 weeks), the patient showed significant regrowth, with visible pigmented terminal hairs and reduction in patch size. Treatment was continued with IL steroid repetition and topical agents.
Treatment Response
- Rapid response: Visible improvement within 4 weeks
- Hair quality: Pigmented terminal hairs (not vellus)
- Patch size reduction: Significant decrease in alopecic area
- Patient satisfaction: Marked improvement in confidence and social comfort
Clinical Implications
This case highlights:
- Fast and robust response to intralesional steroids in localized BAA
- Importance of a tiered treatment plan, escalating only when needed
- Psychological relief achieved through early regrowth
- Role of patient counselling, given AA's unpredictable course
BAA often responds better than scalp AA, making early IL steroids the first-line gold standard.
Conclusion
This case demonstrates successful early intervention in beard alopecia areata using a combination of intralesional steroids, topical immunomodulators, and short-course oral pulse therapy. Substantial improvement within a month underscores the value of multi-modality treatment and regular follow-up.
For resistant disease, advanced options such as excimer laser, contact immunotherapy, and JAK inhibitors remain powerful alternatives.
Learn About Our PRP Hair Treatment